In August the University of South Carolina Columbia campus will welcome students back for the Fall semester. I will be there to welcome them. That is not an extraordinary sentence in most times, but, as we have all become sick of hearing, these are not most times.
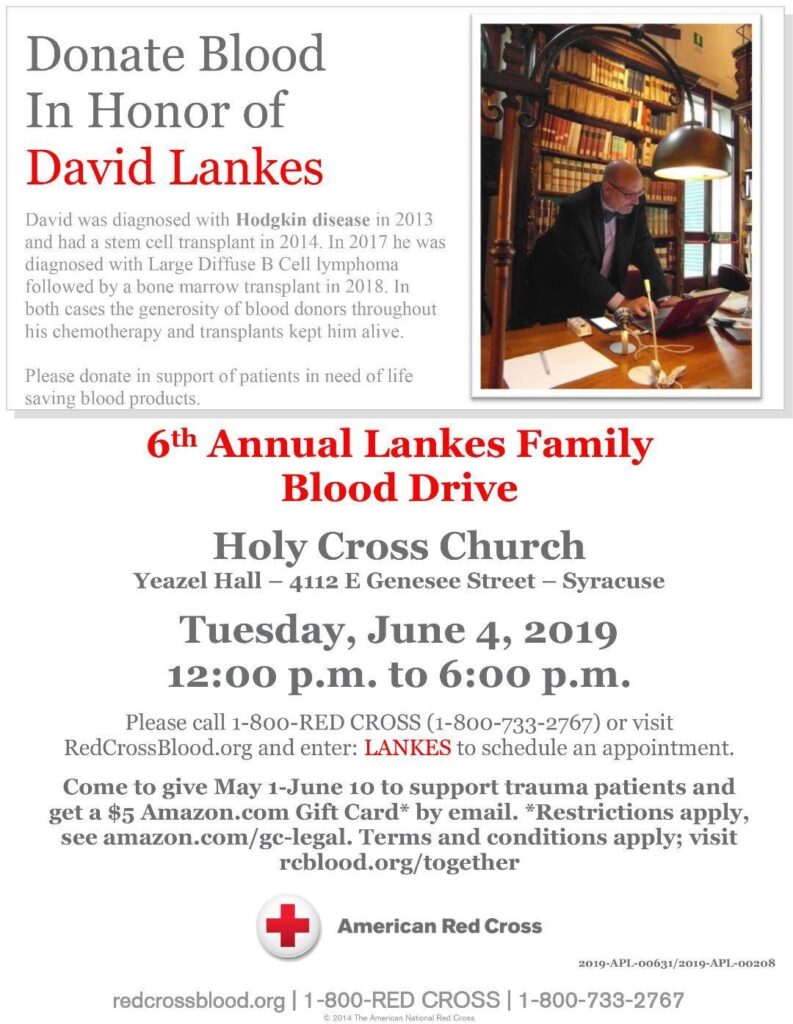
You see, I have every reason not to be there. A new cancer diagnosis in 2017 led to a second bone marrow transplant in 2018. Two years may sound like a long time to recover, but unlike my first bone marrow transplant in 2014, this last one was a donor match and at this point in my recovery my oncologist estimates my immune system at about 25% of normal.
In early March when I asked him what would happen if I contracted the coronavirus his reply was succinct, “you would probably survive, but you would be very sick.” That was early days for this pandemic. His conclusion has not changed.
The university says I don’t have to be there. They have been clear that it is my choice to be on campus, just like it is the choice for students, staff, and faculty. I very much appreciate that choice. But, I will still be there.
The class I will be teaching is online. All of our graduate classes are, and our faculty teaching our undergraduate classes have plenty of experience teaching online. Looking at the teaching evaluations from this last semester, one might ask “what pandemic?” No scores were out of line with previous semesters. In the dozens of classes I looked at I found 4 mentions of moving online – and the only negative one was about how this student wished non-iSchool classes went as smoothly. My faculty doesn’t need me to help them in their classes. But I will still be there.
I love my job because of the people I work with. Staff and faculty left offices over spring break and haven’t been back since. However, not for one minute has the work of the school lagged or been derailed. GoToMeeting, emails, texts, and phone calls have demonstrated that my staff can do their work remotely and well. My staff doesn’t need me there to monitor them. But I will still be there.
I will be there wearing a mask. I will be there with hand sanitizer at the ready. I will wipe surfaces. I will stand 6 feet apart. I will be there because I am asking people I am responsible for to be there if they so choose. I will be there because I would never ask someone to do what I am unwilling to do.
This may seem like a lot of bluster for “so you’re going to do your job?” I get it. But the reason I write this is because we are at a very vulnerable point. A point of closing optimism.
I wrote on April 30 about a New Normal Agenda for Libraries in which I called upon all of us to help create an optimistic new normal for our communities. To ensure that a post-pandemic world was better than before – founded on correcting the fractures and disparities put on vivid display by this crisis: Truly bridging a digital divide where the internet is a utility for all. Working to reform a copyright system based on profit over knowledge creation. Expanding democratic participation, workforce preparation, and standing ready in times of crisis.
In literally the two weeks since I wrote that I have seen a rise of conspiracy theories and denying the very trauma we are living through. I have seen armed protestors defining liberty in the absence of personal and social responsibility. I have seen old political divisions intent on scoring points and raising poll numbers in the face of a generational wakeup call that screams for unity. I have seen times that try a world’s soul result not in calls for cooperation and equity, but in heated arguments on who can make who wear a God damned mask at Costco. Wear a God damned mask.
It has been a dark two weeks for me. And then I began to talk with librarians either opening their libraries or developing plans to do so. I have seen the Facebook posts and Tweets and petitions that libraries should just remain closed and there is no safe way to open. I get it. I would like to agree. To be clear I do agree that simply reopening libraries as they were in some sense of vocational awe or moral obligation is wrong. But that’s not what the librarians I have been talking to, watching, working with are doing. What these folks have shown me is that optimism without pragmatism is as empty as liberty without sacrifice. To get to that New Normal agenda, we have some hard and frankly frightening, and dangerous work to do. Not just in libraries or universities, but across the country.
The librarians I have been talking to are not only fully aware of the risks of opening, even for limited service, they are driven by it. The plans they have shared and put in place, often as a direct response to larger municipal and state mandates, are thoughtful, and, most importantly, collaboratively developed. They have been built on CDC guidelines. WHO guidelines. Guidance from universities. They have been reviewed, amended, and approved by unions, staff, and public health officials. They minimize contact between member and staff, between staff and staff, between staff and materials. They require social distancing, personal protective equipment, and security – like physical security for those who feel their right to infect others outweighs their responsibilities to wear a mask. They have circuit breaker provisions that close services and protect library workers in case of new outbreaks. They make provisions for high risk employees. And to a one, they include shared risk by all levels of an organization. All of them also continue to drive innovation and true community-centered virtual service that continues to demonstrate that libraries are about communities not just things we can loan out.
The reason I am writing this, sharing this, is because these conversations have shown me that my unique and privileged position requires me to be on the record. If those that I educate and collaborate with are required to state their position, then I am so obligated. Just as if I am going to support my university reopening the campus, I am obligated to risk my own health and be there (and work like hell to keep myself and everyone else healthy).
Here’s what we know. The virus is not going away. Sheltering at home flattened a curve and continuing evidence-based hygiene and social distancing precautions saves lives. We need massive, cheap, quick, and readily available testing now everywhere. Even when a vaccine is developed, it will have to overcome a number of obstacles, not the least of which is an anti-vaxxer movement that by all rights should simply disappear in the face of a global pandemic. We know that this pandemic and the resulting economic collapse has put our most vulnerable citizens, especially people of color and the poor at greatest risk. And we know that professionals dedicated to increasing societal knowledge and equity are vital not just online, but in the trenches. We also know that a second wave of infection is likely and we cannot be rash and undo the sacrifice of the past months.
But here’s what else I know. I know that the point of closing optimism must became the point of opening pragmatism or it became the moment of despair. I know that what frightens me more than the virus is a return to a nation divided, unresponsive to those in need, and all too often given to willful ignorance.
Some will criticize me for calling for a cautious reopening. I respect their opinion and continue to be open to conversation. If nothing else I hope this post shows my thinking and continued evolution on the topic. I know some may take these words as a sort of call for removing all restrictions or as a belief that everything is safe now – don’t. Such a reading is just dishonest at best. Let us all acknowledge the complexity of this situation and not be drawn into the trap of flattening narratives into right and wrong, good and bad, open and close. It was that thinking that got us here to begin with.
If you can stay home, for God’s sake stay home. If you have to go out to feed your family, to get medical treatment, to ensure our society still functions, please do so safely. If you don’t need that book, don’t do curbside pickup. If you learn well online, don’t come to campus. If you need to protest, wear a mask not a gun. But if you need a place to sleep or to get out of a dangerous home situation, or for your well-being you need to connect to people in md-August, I’ll be there to open the doors. If you need to connect to the internet to continue your education or keep your job or keep our government accountable, I’ll be there pushing for a new normal.